Skin Care
Dermatologist-Approved Skincare Routine For Pune’s Weather
Pune is situated on the Deccan Plateau, and has a unique climate. The variety of seasons and pleasant temperatures make Pune an ideal city. Thanks to the proximity to the Western Ghats, Pune gets monsoon showers, refreshing winters and warm summers, adding to its lively season cycle. How Does Pune...
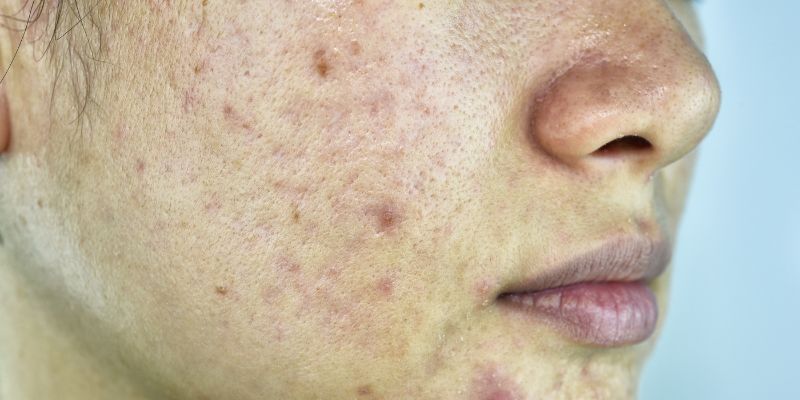
Acne/Pimple Treatment Cost In India – Detailed Price List
Acne is a skin concern that affects men and women of all ages and causes permanent damage if left untreated. Knowing how much acne treatments cost will help you make an informed decision. In India, the average acne treatment costs around INR 2500* per session. Keep reading to learn about...
Laser Hair Removal Cost In Bangalore
Oliva Skin and Hair Clinic offers state-of-the-art laser hair removal treatment in Bangalore with the help of experienced dermatologists who create packages tailored to your individual requirements. We have 7 laser treatment equipped clinics located at Indira Nagar, Whitefield, HRBR Layout, HSR Layout, Jayanagar, Koramangala and Sadashivanagar. What Is Laser...
How to Treat an Infected Pimple
Infected pimples can be stubborn and often more prominent than regular ones. They get swollen and inflamed and require dedicated treatment. Infected pimples are more common among young adults during puberty. The best thing to do when you experience them is to consult a dermatologist as soon as you can....
How to Treat Pimples on the Lips?
Have pimples on your lips and wondering why they occur? You’re not alone! It’s not unusual to get pimples on your lips - like other pimples or acne, clogged pores can cause lip pimples too. While some disappear on their own, some can get severe and leave scars. This article...
How To Get Rid Of Boxcar Scars?
There are different types of acne scars and each of them requires a unique treatment plan. Boxcar scars, which appear as circular or oval depressions on your skin, are the 2nd most common type of atrophic scars after ice pick scars. Atrophic scars are the type where your skin doesn’t...
How To Treat Acne Around the Mouth?
Experiencing acne around the mouth is painful and most of us want to get rid of it at the earliest as it affects our appearance adversely. While there is no singular cause for this, certain skincare products may induce acne. Those having recurring acne around the mouth, chin and lips...
Can Dermal Fillers Help Reverse Acne Scars?
Concealing acne scars can get tiresome. While dealing with acne is one thing, the scars they leave behind are another concern. However, there is a solution for reducing acne scars through advanced fillers. This article will teach you how dermal fillers can reduce acne scars and enhance overall appearance. What...
How To Get Rid Of Fungal Acne?
If your acne is persistent and unresponsive to treatments, then it is likely fungal acne. It differs from the common type of pimples, acne vulgaris, and thus requires an expert diagnosis. There are several ways to prevent it and specific treatments to get rid of it. Learn all that you...
How To Reduce Acne Redness?
While pimples are a common skin concern, redness that occurs as an aftermath of pimples is often ignored. Timely treatment of acne redness is critical to safeguard your skin from future scarring or post-inflammatory hyperpigmentation. There are several ways to effectively treat acne redness. Keep reading to learn about the...